Monitoring Patients Who Are Starting HCV Treatment, Are on Treatment, or Have Completed Therapy
Monitoring Patients Who Are Starting HCV Treatment, Are on Treatment, or Have Completed Therapy
This section provides guidance on monitoring patients with chronic hepatitis C virus (HCV) infection who are starting direct-acting antiviral (DAA) treatment, are on treatment, or have completed therapy. It is divided into 4 parts: pretreatment and on-treatment monitoring (including patients with incomplete adherence); posttreatment follow-up for persons in whom treatment failed to clear the virus; posttreatment follow-up for those who achieve a sustained virologic response (SVR; virologic cure); and additional considerations if treatment includes ribavirin.
Pretreatment and On-Treatment Monitoring
Recommended Assessments Prior to Starting DAA Therapy |
|
|---|---|
| RECOMMENDED |
RATING |
|
Staging of hepatic fibrosis is essential prior to HCV treatment (see Testing and Linkage to Care and see When and in Whom to Treat).
Assessment of potential drug-drug interactions with concomitant medications is recommended prior to starting DAA therapy and, when possible, an interacting co-medication should be stopped or switched to an alternative with less risk for potential interaction during HCV treatment. (See Table of Drug Interactions with Direct-Acting Antivirals and Selected Concomitant Medications below or use an online resource such as University of Liverpool interaction checker.)
Patients should be educated about the proper administration of DAA medications (eg, dose, frequency of medicines, food effects, missed doses, adverse events, etc), the crucial importance of adherence, and the need to inform the healthcare provider about any changes to their medication regimen.
|
I, C |
| The safety of ribavirin-free DAA regimens in humans has not been established during pregnancy and for nursing mothers, so counseling should be offered to women of childbearing age before beginning HCV treatment. (See ribavirin pregnancy recommendations below.) | I, C |
| All patients initiating DAA therapy should be assessed for active hepatitis B virus (HBV) coinfection with HBV surface antigen (HBsAg) testing, and for evidence of prior infection with HBV core antibody (anti-HBc) and HBV surface antibody (anti-HBs) testing. | IIa, B |
| Patients found or known to be HBsAg-positive should be assessed for whether their HBV DNA level meets AASLD criteria for HBV treatment and initiation of antiviral therapy for HBV. | Strong, Moderatea |
| All patients should be assessed for HIV coinfection prior to initiating DAA therapy. | IIa, B |
| Testing for the presence of resistance-associated substitutions (RASs) prior to starting treatment should be performed as recommended in the Initial Treatment and the Retreatment sections. Additional information about RAS testing can be found in the HCV Resistance Primer. | IIb, B |
Patients scheduled to receive an HCV NS3 protease inhibitor (ie, grazoprevir, voxilaprevir, glecaprevir) should be assessed for a history of decompensated liver disease and liver disease severity using the Child-Turcotte-Pugh (CTP) score (see third-party calculator).
|
I, A |
| a Unlike the AASLD/IDSA HCV guidance, the AASLD guidelines for treatment of chronic hepatitis B uses the GRADE system to rate recommendations; please see that document for further information about this rating system. | |
Recommended Monitoring During Antiviral Therapy |
|
|---|---|
| RECOMMENDED |
RATING |
| Clinic visits or telephone contact are recommended as clinically indicated during treatment to ensure medication adherence and monitor for adverse events and potential drug-drug interactions (see table of Drug Interactions with Direct-Acting Antivirals and Selected Concomitant Medications below), especially with newly prescribed medications. | I, B |
| Inform patients taking diabetes medication of the potential for symptomatic hypoglycemia. On-treatment and posttreatment monitoring for hypoglycemia is recommended. | I, C |
| Inform patients taking warfarin of the potential for changes in their anticoagulation status. On-treatment and posttreatment INR monitoring for subtherapeutic anticoagulation is recommended. | I, C |
|
Patients receiving elbasvir/grazoprevir should be monitored with a hepatic function panel at 8 weeks and again at 12 weeks if receiving 16 weeks of treatment. |
I, B |
|
A ≥10-fold increase in ALT values from baseline at any time during treatment should prompt discontinuation of DAA therapy (especially with signs or symptoms of liver inflammation or increasing conjugated bilirubin, alkaline phosphatase, or INR).
An increase in ALT <10-fold from baseline that is accompanied by any weakness, nausea, vomiting, jaundice, or significantly increased bilirubin, alkaline phosphatase, or INR should also prompt discontinuation of DAA therapy. Asymptomatic increases in ALT <10-fold from baseline should be closely monitored with repeat testing at 2-week intervals. If levels remain persistently elevated, consideration should be given to discontinuation of DAA therapy. |
I, B |
|
Quantitative HCV viral load testing is recommended 12 or more weeks after completion of therapy to document sustained virologic response (SVR), which is consistent with cure of chronic HCV infection. |
I, B |
For HBsAg-positive patients not already receiving HBV suppressive therapy because their baseline HBV DNA level does not meet treatment criteria, one of two approaches may be taken:
|
IIa, B |
The recommended pretreatment testing assumes that a decision to treat with antiviral medications has already been made and that the testing involved in deciding to treat—including testing for HCV genotype and assessment of hepatic fibrosis—has already been completed (see When and in Whom to Initiate HCV Therapy).
Prior to starting treatment, patients should be evaluated for potential drug-drug interactions with selected antiviral medications by consulting the prescribing information and using other resources (eg, http://www.hep-druginteractions.org). The table below lists known drug-drug interactions between HCV DAAs and selected medications.
Table. Drug Interactions with Direct-Acting Antivirals and Selected Concomitant Medications
| Concomitant Medications | SOF/VEL | GLE/PIB | SOF/VEL/VOX | LDV/SOF | EBR/GZR |
|---|---|---|---|---|---|
| Acid-reducing agents |
Antacids H2RA PPI |
H2RA PPI |
Antacids H2RA PPI |
Antacids H2RA PPI |
|
| Alpha-1 blockers |
Prazosin Silodosin |
Prazosin Silodosin |
Prazosin Silodosin |
Silodosin |
Prazosin Silodosin |
| Analgesics | Metamizole |
Alfentanil |
Metamizole |
Fentanyl |
|
| Antiarrhythmics |
Amiodarone Dronedarone |
Amiodarone |
Amiodarone Dronedarone |
Amiodarone Dronedarone |
Amiodarone Dronedarone Quinidine |
|
Digoxin Quinidine |
Digoxin Quinidine |
Digoxin Quinidine |
|||
| Anticoagulant and antiplatelet agents |
Apixaban Dabigatran Edoxaban Rivaroxaban Ticagrelor Warfarin |
Dabigatran |
Dabigatran Edoxaban |
Apixaban Dabigatran Edoxaban Rivaroxaban Ticagrelor Warfarin |
Apixaban Dabigatran Edoxaban Rivaroxaban Ticagrelor Warfarin |
|
Apixaban Edoxaban Rivaroxaban Ticagrelor Warfarin |
Apixaban Rivaroxaban Ticagrelor Warfarin |
||||
| Anticonvulsants and barbiturates |
Amobarbital Carbamazepine Eslicarbazine Oxcarbazepine Phenobarbital Phenytoin Primidone |
Amobarbital Carbamazepine Eslicarbazine Oxcarbazepine Phenobarbital Phenytoin Primidone |
Amobarbital |
Amobarbital Carbamazepine Oxcarbazepine Phenobarbital Phenytoin Primidone |
Amobarbital Carbamazepine Eslicarbazine Oxcarbazepine Phenobarbital Phenytoin Primidone |
| Rufinamide | Rufinamide | Rufinamide | Rufinamide Zonisamide | Rufinamide | |
| Antihypertensives | Diltiazem | Aliskiren |
Aliskiren Enalapril Irbesartan Isradipine Non-DHP CCB Olmesartan Telmisartan Valsartan |
Aliskiren Amlodipine Diltiazem Eplerenone Felodipine Irbesartan Isradipine |
Eplerenone Felodipine Isradipine |
|
Enalapril Eplerenone Irbesartan Isradipine Non-DHP CCB Olmesartan Telmisartan |
|||||
| Antimycobacterials |
Rifabutin |
Rifabutin |
Rifabutin |
Bedaquiline |
Rifabutin |
|
Bedaquiline |
Rifabutin |
Bedaquiline |
|||
| Antipsychotics – first generation | Pimozide | Pimozide | Pimozide | ||
|
Droperidol Thioridazine |
|||||
| Antipsychotics – second generation |
Aripiprazole Clozapine Paliperidone Quetiapine |
Paliperidone | Paliperidone |
Aripiprazole Quetiapine |
|
| Antiretrovirals | See HIV/HCV Coinfection Section | ||||
| Azole antifungals |
Ketoconazole Posaconazole |
Ketoconazole | |||
| Benzodiazepines | Midazolam | ||||
|
Bronchodilators |
Theophylline | ||||
| Buprenorphine/ naloxone | |||||
| Calcineurin inhibitors |
Cyclosporine |
Cyclosporine | Cyclosporine | ||
| Tacrolimus | Tacrolimus | ||||
| Cancer Therapies |
Acalabrutinib |
Acalabrutinib |
Acalabrutinib |
Acalabrutinib |
Acalabrutinib |
|
Vinblastine |
Imatinib |
||||
| Cholesterol-lowering agents |
Atorvastatin Fluvastatin Lovastatin Pitavastatin Rosuvastatin Simvastatin |
Atorvastatin Lovastatin Simvastatin |
Atorvastatin Fluvastatin Lovastatin Pitavastatin Rosuvastatin Simvastatin |
Rosuvastatin |
Atorvastatin Fluvastatin Gemfibrozil Lovastatin Rosuvastatin Simvastatin |
|
Ezetimibe Fluvastatin Gemfibrozil Pitavastatin Pravastatin Rosuvastatin |
Ezetimibe |
Atorvastatin Fluvastatin Lovastatin Pitavastatin Pravastatin Simvastatin |
|||
| Cisapride | |||||
| COVID-19 antivirals |
Molnupiravir |
Molnupiravir |
Molnupiravir |
Molnupiravir |
Molnupiravir |
|
Nirmatrelvir/ |
Nirmatrelvir/ |
Nirmatrelvir/ |
|||
| Ergot derivatives | |||||
| Ethinyl estradiol containing products | |||||
| Glucocorticoids | Dexamethasone | Dexamethasone | Dexamethasone | ||
| Heart failure agents | Bosentan | Bosentan | Bosentan | Bosentan | |
| Ambrisentan | Ambrisentan | Ambrisentan | |||
| Herbals | St. John’s wort | St. John’s wort | St. John’s wort | St. John’s wort | St. John’s wort |
| Loop diuretics | |||||
| Macrolide antimicrobials | Troleandomycin |
Erythromycin Telithromycin |
Erythromycin Telithromycin |
Telithromycin | Telithromycin |
| Troleandomycin | Troleandomycin | Troleandomycin | |||
| Phosphodiesterase-5 inhibitors | |||||
| Recreational Drugs |
Carfentanil |
Carfentanil |
|||
|
H2RA=Histamine H2 Antagonist; PPI=proton pump inhibitor; DHP CCB=dihydropyridine calcium channel blocker; Non-DHP CCB=non dihydropyridine calcium channel blocker. Green indicates coadministration is safe; yellow indicates a dose change or additional monitoring is warranted; and red indicates the combination should be avoided. Specific concomitant medications or medication classes with actual or theoretical potential for interaction are listed in the box. |
|||||
The education of patients and caregivers about potential adverse effects of DAA therapy and their management is an integral component of treatment and is important for a successful outcome in all patient populations. During DAA treatment, individuals should be followed at clinically appropriate intervals to ensure medication adherence, assess adverse events and potential drug-drug interactions, and monitor blood test results necessary for patient safety. This includes on-treatment and posttreatment monitoring for hypoglycemia or subtherapeutic INR levels among patients taking diabetes medicines or warfarin, respectively. Real-world data indicate an association between DAA therapy and related changes in hepatic function and alterations in dose-response relationships with these medications (Drazilova, 2018); (Abdel Alem, 2017); (Rindone, 2017); (Pavone, 2016); (DeCarolis, 2016); (Soriano, 2016). Inform patients on these medications about the potential for these developments; make dose adjustments as needed. The frequency and type of contact (eg, clinic visit, phone call, etc) are variable but need to be sufficient to assess patient safety and response to treatment, as outlined above.
Routine testing for HCV RNA during treatment is not recommended unless the ALT level fails to decline (when elevated) or there are concerns regarding patient adherence with DAA treatment. There are no data to support stopping treatment based on detectable HCV RNA during the first 4 weeks of treatment, or that detectable HCV RNA at this time point signifies medication nonadherence.
It is essential to test for HCV RNA 12 weeks (or longer) after treatment completion. Undetectable or unquantifiable HCV RNA 12 weeks or longer after treatment completion is defined as a sustained virologic response (SVR), which is consistent with cure of chronic HCV infection. Virologic relapse is rare 12 weeks or longer after treatment completion (Sarrazin, 2017); (Simmons, 2016). Nevertheless, repeat quantitative HCV RNA testing can be considered at 24 or more weeks after completing treatment for patients in whom ALT increases to above the upper limit of normal.
During clinical trials with elbasvir/grazoprevir, with or without ribavirin, 1% of participants experienced ALT elevations from normal levels to >5 times the upper limit of normal, generally at or after treatment week 8. ALT elevations were typically asymptomatic, and most resolved with ongoing therapy or completion of therapy. Higher rates of late ALT elevations occurred in females, those of Asian descent, and patients aged ≥65 years. Hepatic laboratory testing should be performed prior to therapy, at treatment week 8, and as clinically indicated. For patients receiving 16 weeks of therapy, additional hepatic laboratory testing should be performed at treatment week 12 (Zepatier package insert, 2019).
One recent cohort study of 18,498 initiators of PI-based DAA therapy (paritaprevir/ritonavir/ombitasvir +/- dasabuvir, elbasvir/grazoprevir, glecaprevir/pibrentasvir) matched 1:1 on propensity score to non-PI-based DAA initiators (ledipasvir/sofosbuvir, sofosbuvir/velpatasvir) was conducted within the US Veterans Health Administration from 2014-2019 (Torgersen, 2021). During exposure to DAA therapy, the study determined incident development of: 1) ALT >200 U/L, 2) severe hepatic dysfunction (defined by coagulopathy with hyperbilirubinemia), and 3) hepatic decompensation, according to baseline FIB-4 score (≤3.25; >3.25). The analysis found that the risk of incident ALT elevations was increased among PI-based DAA initiators in both FIB-4 groups, but the risk of severe hepatic dysfunction or hepatic decompensation did not differ between PI and non-PI-based DAA initiators in either FIB-4 group.
Patients being treated with amiodarone should not receive sofosbuvir-based regimens due to risk of life-threatening arrhythmias. Because of its long half-life, it is advised that persons should be off amiodarone for at least 6 months before initiating sofosbuvir. If the decision is made to start sofosbuvir in this setting, continued vigilance for bradycardia should be exercised.
Simplified HCV Treatment for Treatment-Naïve Adults
Recent data from a global sample of patients undergoing antiviral treatment for chronic HCV infection suggested that a minimal monitoring approach was safe and achieved SVR at a rate comparable to that with standard monitoring. This minimal monitoring approach was examined in a phase 4, open label, single-arm trial that enrolled 400 treatment-naïve patients 18 years or older with HCV RNA >1,000 IU/mL from Brazil, South Africa, Thailand, Uganda, and the USA with capped inclusion of compensated cirrhosis and HIV/HCV coinfection (Solomon, 2022). Pregnancy, breastfeeding, or evidence of chronic hepatitis B virus (HBV) infection (HBsAg-positive) were exclusion criteria; however, participants with resolved HBV infection (hepatitis B core total antibody [anti-HBc] with or without positive hepatitis B surface antibodies [anti-HBs]) were eligible. Patients initiated treatment with fixed dose sofosbuvir (400 mg)/velpatasvir (100 mg) once daily for 12 weeks. Minimal monitoring involved: 1) no pre-treatment genotyping; 2) dispensing the entire treatment course (84 tablets) at entry; 3) no scheduled visits or laboratory monitoring; and 4) remote contact at week 4 to assess DAA adherence and at week 22 to schedule SVR assessment at week 24.
Of the 400 participants, 399 initiated sofosbuvir/velpatasvir treatment. At entry, 166 (42%) were living with HIV, 34 (9%) had compensated cirrhosis, and 121 (32%) of 374 with HBV panel (HBsAg, anti-HBc, anti-HBs) available had evidence of resolved HBV infection. Overall, 379 of the 399 who initiated treatment achieved SVR (95.0%; 95% CI, 92.4-96.7%). A total of 14 (4%) of 397 participants reported serious adverse events between treatment initiation and week 28, but none were treatment-related or led to treatment discontinuation or death. Because of the possible risk for HBV reactivation that could be fulminant, these HBV-HCV co-infected patients should be excluded.
Given the findings of this minimal monitoring study, simplified HCV treatment approaches are available for HCV treatment-naïve adults without cirrhosis (click here) and for HCV treatment-naïve adults with compensated cirrhosis (click here).
Pregnancy and Nursing Mothers
Few adequate and well-controlled human studies are available to establish whether DAAs pose a risk to pregnancy outcomes or whether DAAs and their metabolites are present in breastmilk. An open-label, phase 1 study of HIV-negative pregnant women with chronic genotype 1 infection evaluated a 12-week course of ledipasvir/sofosbuvir initiated between 23 to 24 weeks of gestation (Chappell, 2019). Among 7 evaluable patients, all achieved SVR12; adverse events related ledipasvir/sofosbuvir were ≤ grade 2. All 7 participants delivered at term with undetectable HCV viral loads at delivery. One-year follow-up of the infants is ongoing.
Given the dearth of data on this topic, clinicians should discuss with female patients that DAAs should be used during pregnancy only if the potential benefit of DAA therapy justifies the potential risk of harm to the fetus. The health benefits of DAA therapy for nursing mothers should be weighed against the health benefits of breast feeding and the possible adverse effects of the DAA regimen on the breastfed child. Given the relatively short duration of treatment and the availability of ribavirin-free regimens in most patients, the potential risk of harms and benefits of delaying pregnancy until HCV DAA therapy is completed should be considered. For additional information about HCV and pregnancy, click here.
Reactivation of Hepatitis B Virus Infection
Cases of hepatitis B virus (HBV) reactivation, occasionally fulminant, during or after DAA therapy have been reported in HBV/HCV coinfected patients who were not receiving HBV suppressive therapy (Mücke, 2018); (Bersoff-Matcha, 2017); (Chen, 2017). Therefore, all patients initiating DAA therapy should be assessed for HBV coinfection with HBsAg testing, and for evidence of prior infection with anti-HBc and anti-HBs testing. HBV vaccination is recommended for all susceptible individuals. Testing for HBV DNA should be performed prior to DAA therapy in patients who are HBsAg positive. HBsAg-positivity does not represent a contraindication to DAA therapy. Patients meeting criteria for treatment of active HBV infection should be started on HBV therapy at the same time or before DAA therapy is initiated (Terrault, 2018).
Patients with a low or undetectable HBV DNA level can either receive prophylactic HBV treatment for the duration of DAA treatment until assessment for SVR12 or be monitored at regular intervals (usually not more frequently than every 4 weeks) for HBV reactivation with HBV DNA testing. If monitoring is elected, HBV treatment should be started if the HBV DNA level increases >10-fold or is >1000 IU/mL in a patient with undetectable or unquantifiable HBV DNA prior to DAA treatment. There are insufficient data to provide clear recommendations for the monitoring of HBV DNA among patients testing positive either for anti-HBc alone (isolated anti-HBc) or for both anti-HBc and anti-HBs (resolved infection). However, the possibility of HBV reactivation should be considered in these patients in the event of an unexplained increase in liver aminotransferase levels during and/or after completion of DAA therapy.
Posttreatment Follow-Up for Patients in Whom Treatment Failed
Recommended Monitoring for Patients in Whom Treatment Failed to Achieve a Sustained Virologic Response |
|
|---|---|
| RECOMMENDED |
RATING |
| Retreatment for chronic HCV is recommended utilizing the regimens recommended in the Retreatment section. | I, C |
| Disease progression assessment every 6 to 12 months with a hepatic function panel, complete blood count (CBC), and international normalized ratio (INR) is recommended if patients are not retreated or fail a second or third DAA treatment course. | I, C |
| Surveillance for hepatocellular carcinoma with liver ultrasound examination, with or without alpha fetoprotein (AFP), every 6 months is recommended for patients with cirrhosisa in accordance with the AASLD guidance on the diagnosis, staging, and management of hepatocellular carcinoma. | Low, Conditionalb |
| For patients with cirrhosis, endoscopic surveillance for varices should be performed in accordance with the AASLD guidance on portal hypertension bleeding in cirrhosis. | Guidanceb |
|
a For decompensated cirrhosis, please refer to the appropriate section. b Unlike the AASLD/IDSA HCV guidance, the AASLD guidelines use the GRADE system to rate recommendations; please see that document for further information about this rating system. |
|
The Following Monitoring Is Not Recommended During or After Therapy |
|
|---|---|
| NOT RECOMMENDED |
RATING |
| Monitoring for HCV drug resistance-associated substitutions (RASs) during or after therapy is not recommended unless retreatment will be performed. RAS testing is recommended in advance of retreatment therapy. See the Retreatment section for recommendations regarding RAS testing prior to retreatment. Additional information about RAS testing can be found in the HCV Resistance Primer. | IIb, C |
Patients who do not achieve SVR retain the possibility of continued liver injury, progression of hepatic fibrosis, and the potential to transmit HCV infection to others. Such patients should be considered for retreatment per the Retreatment of Persons in Whom Prior Therapy Has Failed section.
Given that persons in whom treatment failed remain at risk for ongoing liver injury and liver fibrosis progression (Dienstag, 2011), these patients should be monitored for signs and symptoms of decompensated cirrhosis. Patients in whom antiviral therapy failed may harbor viruses that are resistant to one or more of the antivirals at the time of virologic breakthrough (Lawitz, 2014a); (Schneider, 2014). There is no evidence to date, however, that the presence of resistance-associated substitutions (RASs) results in more progressive liver injury than would have occurred if the patient did not have resistant viruses. Additional information about RASs and RAS testing can be found in the HCV Resistance Primer section. If there remains uncertainty regarding the applicability of RAS testing, consultation with an expert regarding the treatment of HCV infection may be useful.
Posttreatment Follow-Up for Patients Who Achieved a Sustained Virologic Response
Recommended Follow-Up for Patients Who Achieved a Sustained Virologic Response (SVR) |
|
|---|---|
| RECOMMENDED |
RATING |
| For noncirrhotic patients, recommended follow-up is the same as if they were never infected with HCV. | I, B |
| Assessment for HCV recurrence is recommended only if the patient develops unexplained hepatic dysfunction, or annual assessment if the patient has ongoing risk factors for HCV infection. In such cases, a quantitative HCV-RNA test rather than an HCV-antibody test is recommended to assess for HCV recurrence. | I, A |
| Surveillance for hepatocellular carcinoma is recommended for patients with cirrhosis,a in accordance with the AASLD guidance on the diagnosis, staging, and management of hepatocellular carcinoma. | Strong, Moderateb |
| For cirrhotic patients, upper endoscopic surveillance is recommended in accordance with the AASLD guidance on portal hypertension bleeding in cirrhosis. | Guidanceb |
| Assessment for other causes of liver disease is recommended for patients who develop persistently abnormal liver tests after achieving SVR. | I, C |
|
a For decompensated cirrhosis, please refer to the appropriate section. b Unlike the AASLD/IDSA HCV guidance, the AASLD guidelines use the GRADE system to rate recommendations; please see that document for further information about this rating system. |
|
Patients with undetectable serum HCV RNA, as assessed by a sensitive polymerase chain reaction (PCR) assay, ≥12 weeks after treatment completion are deemed to have achieved SVR (ie, cure). The likelihood of achieving SVR with DAA therapy among adherent, immunologically competent, treatment-naive patients with compensated liver disease generally exceeds 95%. Among patients who achieved SVR with peginterferon/ribavirin treatment, more than 99% have remained free of HCV infection when followed for 5 years after treatment completion (Manns, 2013). Thus, achieving SVR is considered a virologic cure of HCV infection. SVR typically aborts progression of liver injury with regression of liver fibrosis in most (but not all) treated patients (Morgan, 2013); (Morisco, 2013); (Morgan, 2010); (Singal, 2010); (George, 2009). Liver fibrosis and liver function test results improve in most patients who achieve SVR (Morgan, 2013); (Morisco, 2013); (Morgan, 2010); (Singal, 2010); (George, 2009). Because of lack of progression, noncirrhotic patients who achieve SVR should receive standard medical care that is recommended for patients who were never infected with HCV unless they remain at risk for non-HCV–related liver disease, such as nonalcoholic fatty liver disease or alcoholic liver disease.
Among cirrhotic patients who achieve SVR, decompensated liver disease (with the exception of hepatocellular carcinoma [HCC]) rarely develops during follow-up and overall survival is prolonged (Morgan, 2013); (Morisco, 2013); (Morgan, 2010); (Singal, 2010); (George, 2009). Bleeding from esophageal varices is rare after SVR (Morgan, 2013); (Morisco, 2013); (Morgan, 2010); (Singal, 2010); (George, 2009). Cirrhotic patients should undergo surveillance endoscopy every 2 years if known to have small varices and every 3 years in the absence of known varices in accordance with AASLD guidance on portal hypertension bleeding (Garcia-Tsao, 2017).
Importantly, cirrhotic patients remain at risk for developing HCC and should, therefore, undergo surveillance for HCC every 6 months utilizing ultrasound (with or without AFP testing) despite the lowered risk that results after viral eradication (Marrero, 2018). Although multiple studies of cirrhotic patients who achieved SVR with peginterferon/ribavirin reported a reduction in the risk of developing HCC (Morgan, 2013); (Morisco, 2013); (Morgan, 2010); (Singal, 2010); (George, 2009) and a meta-analysis of persons achieving SVR with DAAs found that the HCC risk did not exceed that seen in patients who experienced SVR with interferon-based treatment after adjustment for baseline risk factors for HCC (Waziry, 2017b), one report found a higher than expected frequency of HCC in patients with HCV-related cirrhosis despite successful DAA treatment (Reig, 2016). However, a prospective observational study of 3045 cirrhotic patients found an adjusted hazard ratio for HCC of 0.57 (95% CI 0.40 to 0.81) following DAA-based therapy, implying a 43% reduction in HCC incidence (Carrat, 2019).
Bleeding from esophageal varices is uncommon after SVR (Morgan, 2013); (Morisco, 2013); (Morgan, 2010); (Singal, 2010); (George, 2009). Nevertheless, patients with compensated cirrhosis who achieve SVR should continue to receive endoscopic surveillance for esophageal varices, in accordance with the AASLD guidance on portal hypertension bleeding (Garcia-Tsao, 2017). Current AASLD recommendations for patients with compensated cirrhosis without known varices is surveillance endoscopy every 2 years if there is evidence of ongoing liver injury from associated conditions, such as obesity or alcohol use, and every 3 years if liver injury is quiescent, such as after alcohol abstinence. Patients with compensated cirrhosis and known varices should undergo surveillance endoscopy annually if there is evidence of ongoing liver injury from associated conditions, such as obesity or alcohol use, and every 2 years if liver injury is quiescent, such as after alcohol abstinence.
Patients in whom SVR is achieved but who have another potential cause of liver disease (eg, excessive alcohol use, metabolic syndrome with or without proven fatty liver disease, or iron overload) remain at risk for hepatic fibrosis progression. It is recommended that such patients be educated about the risk of liver disease and monitored for liver disease progression with periodic physical examination, blood tests, and potentially, tests for liver fibrosis by a liver disease specialist.
Patients who achieve SVR can have HCV recurrence due to reinfection or late relapse (Sarrazin, 2017); (Simmons, 2016). A systematic review suggests 5-year recurrence risks of 1%, 11%, and 15% in low-risk HCV monoinfected, high-risk HCV monoinfected (ie, people who currently or formerly injected drugs, imprisonment, or men who have sex with men [MSM]), and HIV/HCV coinfected patients, respectively (Simmons, 2016). At least annual testing for HCV reinfection among patients with ongoing risk for HCV infection (eg, injection drug use or high-risk sexual exposure) is recommended. A flare in liver aminotransferase levels should prompt immediate evaluation for HCV reinfection (see Management of Acute HCV Infection). Because HCV antibody remains positive in most patients after achieving SVR, testing for HCV recurrence using an assay that detects HCV RNA (ie, quantitative HCV-RNA test) is recommended.
Acute liver injury is common among patients receiving chemotherapy or immunosuppressive agents. Testing for hepatitis viruses should be included in the laboratory assessment of the cause of acute liver injury in these patients. Approximately 23% of patients with active HCV infection—especially those with a hematologic malignancy—experience a flare in their HCV RNA level (>10-fold) during chemotherapy. An ALT level increase is less common and clinical symptoms of hepatitis are uncommon (Torres, 2018). Among patients who have recovered from HCV infection, either spontaneously or with DAA treatment, reactivation of HCV infection (ie, detectable HCV RNA) during chemotherapy is distinctly uncommon and is not anticipated to occur since there is no residual reservoir for the virus. Thus, in this latter group, routine testing for HCV RNA during immunosuppressive treatment or prophylactic administration of antivirals during immunosuppressive treatment is not recommended.
Additional Considerations If Treatment Includes Ribavirin
Ribavirin causes hemolysis. Patients receiving ribavirin should have hemoglobin levels checked during treatment, often after 2 weeks, and the ribavirin dose reduced if the patient develops significant anemia, often defined as hemoglobin <10 g/dL.
Ribavirin causes fetal death and fetal abnormalities in animals. Ribavirin should not be administered to pregnant women or to women who might become pregnant during or for 6 months after completing ribavirin treatment. Similarly, ribavirin may cause birth defects in offspring of women whose partner was receiving ribavirin when the woman became pregnant. In the very rare instances when ribavirin is used, it is imperative for persons of childbearing potential to use at least 2 reliable forms of effective contraception during treatment and for a period of 6 months thereafter. It is recommended that the healthcare practitioner document the discussion of the potential teratogenic effects of ribavirin in the patient’s medical record.
Incomplete Adherence
There are minimal data regarding the outcome of patients who have incomplete adherence to DAA therapy or the threshold level of adherence below which the incidence of SVR12 is significantly reduced. Missing doses of DAAs is relatively common. A secondary analysis of data from electronic blister packs that recorded the date and time of each dose among 103 participants in a velpatasvir/sofosbuvir clinical trial demonstrated that approximately one-third (32%) of study participants had <90% adherence (ie, nonadherence) (Cunningham, 2018). The most common episodes of nonadherence lasted 1–2 days (61% of episodes); 11% of episodes lasted ≥7 days. Despite the nonadherence, SVR12 was 94% among both DAA adherent (≥90% of doses) and nonadherent (<90% of doses) patients. Longer durations of missed treatment, however, may affect SVR. A study of patients receiving DAA treatment found that only 50% (2/4) patients with F0-F3 disease who took <4 weeks of their course of therapy experienced SVR, compared with an SVR of 99% (109/110) for those who received ≥4 weeks of therapy. Among patients with cirrhosis, a lower SVR12 rate was observed in those who took <8 weeks of therapy compared with participants who took ≥8 weeks (83% [25/30] vs 95% [209/221]) (Fabbiani, 2021).
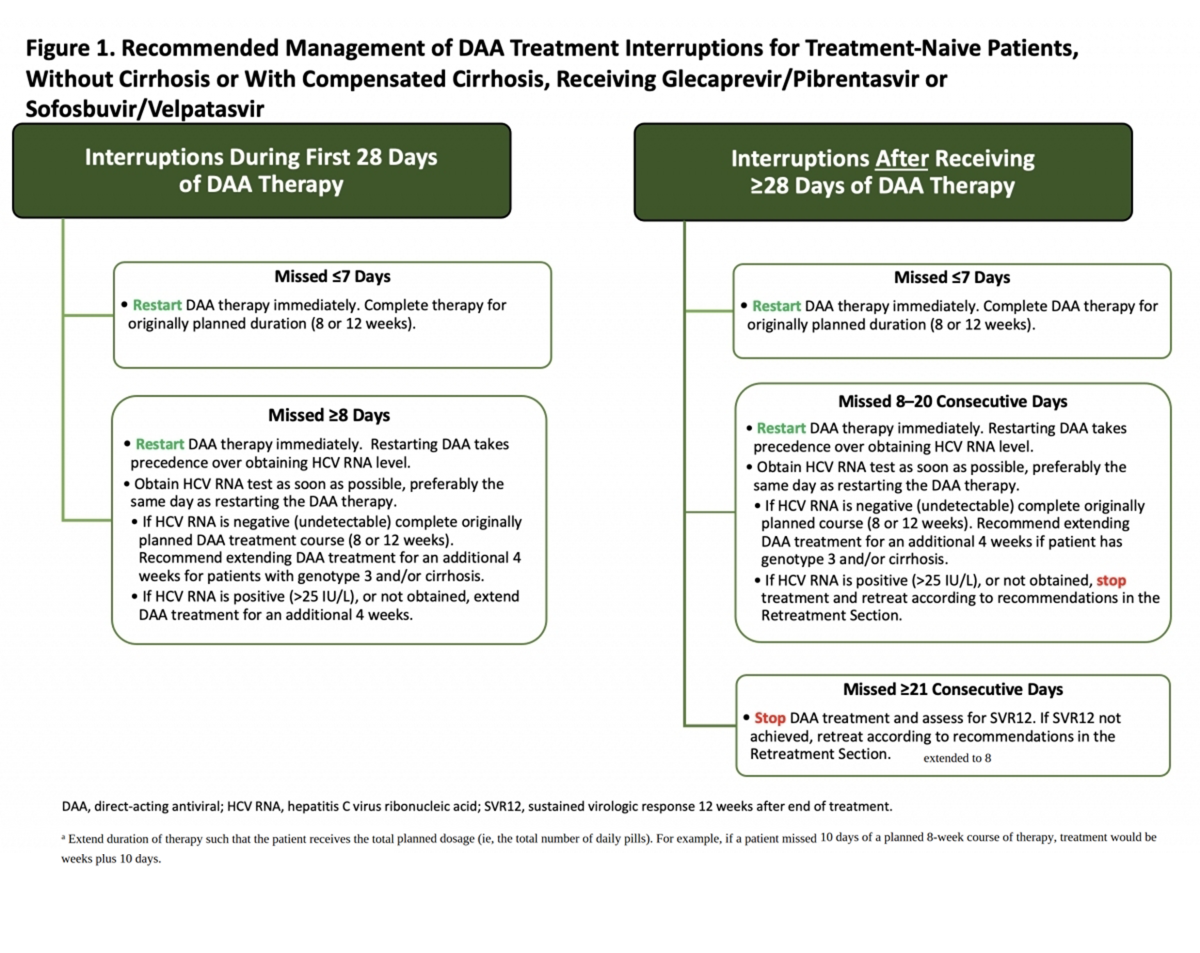
There are few data on which to base recommendations regarding how to manage patients who have discontinued DAAs for several days to weeks. The recommendations shown in Figure 1 are applicable to treatment-naive patients with acute or chronic HCV, without cirrhosis or with compensated cirrhosis, receiving either glecaprevir/pibrentasvir or sofosbuvir/velpatasvir. These recommendations are based on the opinion of the AASLD-IDSA HCV Treatment Guidance Panel.
Patients with prior DAA treatment, or receiving other DAA treatment regimens, or other populations (eg, patients who are posttransplant or have decompensated cirrhosis) should be managed in consultation with an expert. All patients with incomplete adherence should be asked about factors contributing to adherence or nonadherence, and counseled regarding the importance of adherence. In general, the panel considers a treatment interruption of <7 days unlikely to impact SVR12, based on adherence and outcome data from the SIMPLIFY study (Cunningham, 2018).
Click the graphic to enlarge Figure 1.